Osteoarthritis (OA) is the most common form of arthritis. Some people call it degenerative joint disease or “wear and tear” arthritis. It occurs most frequently in the hands, hips, and knees. With OA, the cartilage within a joint begins to break down and the underlying bone begins to change.
WHO states the global incidence of knee OA was 203 per 10,000 person-years (95% CI, 106–331) in individuals aged 20 and over. Correspondingly, there are around annual 86⋅7 (95% CI, 45⋅3–141⋅3) million individuals (20 years and older) with incident knee OA in 2020 worldwide.
Classification
Osteoarthritis is classified into two classifications, yet the distinction between the two of them is always unclear.
- Primary or idiopathic OA has no prior event or disease related to it.
- Secondary OA results from previous joint injury or inflammatory disease.
-
Pathophysiology
Osteoarthritis may be thought of as the result of many factors that, when combined, predispose the patient to the disease.

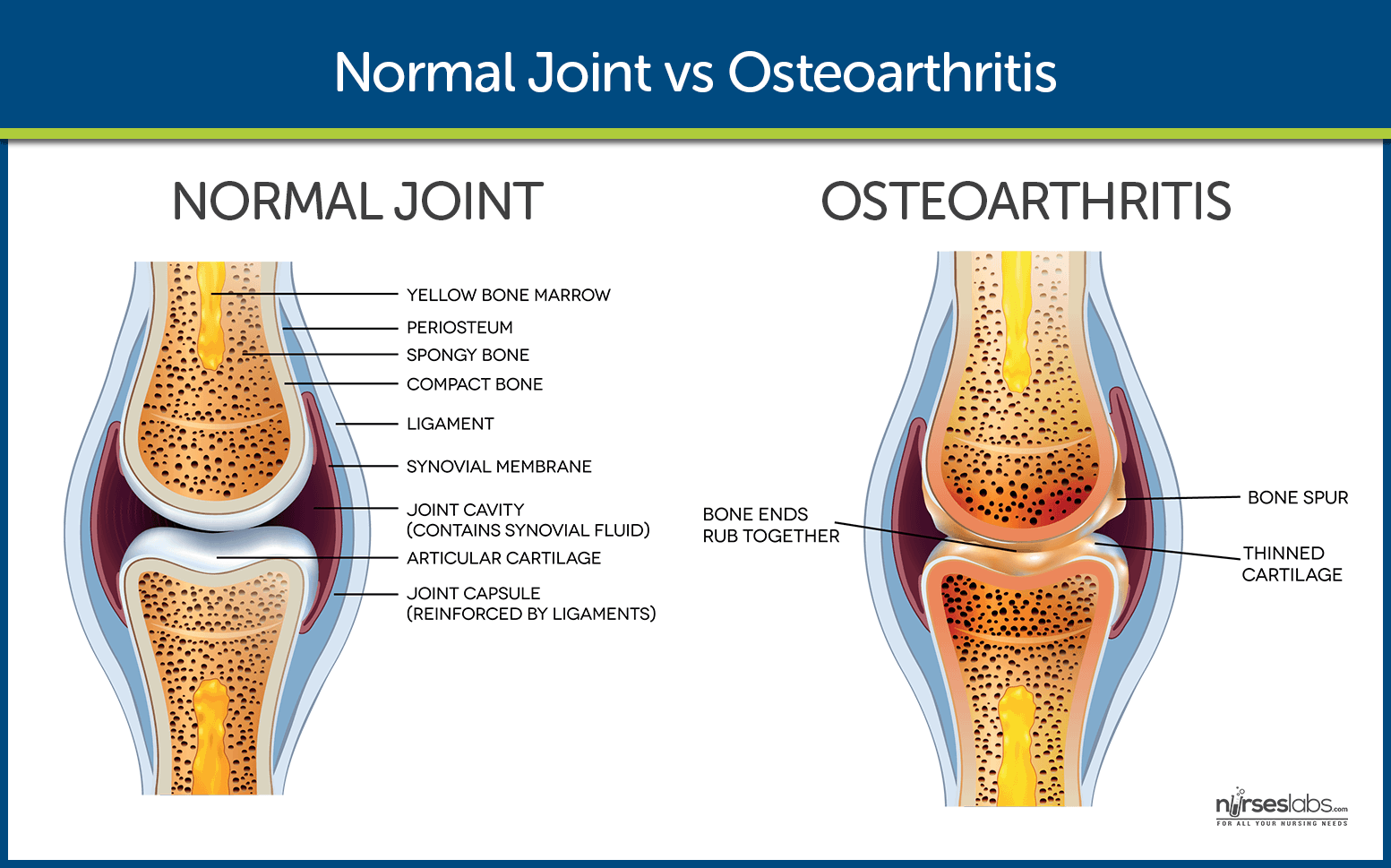
In healthy joints, two bones articulate with one another separated by shock-absorbing cartilage. Both the cartilage and the bone are important in dissipating the load placed through joints every day. When joints are subjected to large loads or impact, the cartilage and bone may be damaged.
Numerous repair mechanisms attempt to restore normal function within the damaged joint to ensure the joint continues to dissipate load correctly. This includes cell-mediated remodeling within the architecture of the cartilage and subchondral bone tissues. When the rate of damage exceeds the rate of repair, degeneration of the bone and cartilage ensues and the joint fails to effectively dissipate load.
This results in a cycle of biomechanical and biochemical degeneration, where the shock-absorbing cartilage is progressively destroyed, exposing the bone to greater load and leading to bone damage (bone marrow lesions). This leads to further loss of cartilage, narrowing of the joint space (the space between the bones) and the overgrowth of bone (osteophyte formation), which causes hard lumps to develop around the joints.
Joint degeneration results in painful and tender inflammation of the synovial lining of the joint (synovitis) and swelling of the joint (effusion). While the cartilage, bone and synovial lining are important tissues, the whole joint is involved in the pathogenesis.
Modern imaging techniques, such as magnetic resonance imaging (MRI), have established that the loss of cartilage, bone marrow lesions and synovitis are common in OA and are predictive factors for requiring a joint replacement. MRI-detected synovitis and bone marrow lesions are also associated with OA pain. Synovitis may be present in early cartilage changes to the joint, and there is cellular infiltration with macrophages, activated T and B cells and accompanying vascular proliferation. Inflammatory cytokine levels may also be elevated in the joint, but to a lesser extent than seen in RA.
Check out this awesome pathophysiology and easy-to-understand video by Osmosis.
Check out this awesome pathophysiology and easy-to-understand video by Osmosis.
Statistics and Epidemiology
Osteoarthritis often begins with the third decade of life and peaks between the fifth and the sixth decades.
- By 40 years of age, 90% of the population has degenerative joint changes in their weight-bearing joints.
- Prevalence of OA is between 50% and 80% in the elderly.
- Increasing age directly relates to the degenerative process in the joint.
Causes of Osteoarthritis in Cameroon
There is no single cause of OA, and the exact etiology of OA is unknown. A combination of factors increase the risk of developing OA. These include:
- Aged over 50 years
- Female sex
- Increased body mass index (BMI>25)
- Previous injury to the affected joint
- Laxity of joint ligaments
- Occupational or recreational use of the affected joint
- Family history.
OA can affect weight-bearing and non-weight-bearing joints, and may involve single or multiple joints. Each of these types of OA have their own risk factors and there is currently no validated risk tool for the quantitative prediction of developing OA.
Sex hormones may influence the development of hand OA among young women. Women younger than 40 years of age have a lower incidence of hand OA compared with men of the same age; however, over the age of 40 years there is a higher incidence in women. However, to date hormone replacement therapy (HRT) studies have not supported this hypothesis, as there was no reduction in hand OA in women who have received HRT. Further research is required to fully evaluate the relationship between female hormones and OA.
Genetic studies have shown that OA is genetically heterogenous, with common gene variants contributing only modestly to the risk of OA. However, studies have suggested there may be genetic variation in the causes of pain among people with OA. The SCN9A gene is responsible for three inherited human pain disorders (primary erythermalgia, paroxysmal extreme pain disorder and channelopathy-associated insensitivity to pain) and variation at this gene affecting peripheral pain thresholds have been implicated in various forms of chronic pain, including in people with OA
Statistics and Epidemiology
Osteoarthritis often begins with the third decade of life and peaks between the fifth and the sixth decades.
- By 40 years of age, 90% of the population has degenerative joint changes in their weight-bearing joints.
- Prevalence of OA is between 50% and 80% in the elderly.
- Increasing age directly relates to the degenerative process in the joint.
Signs and Symptoms of Osteoarthritis
Osteoarthritis has primary signs and symptoms, and that includes:

- Pain. Inflamed synovium causes the pain, stretching of the joint capsule or ligaments, irritation of the nerve endings in periosteum over osteophytes, trabecular microfracture, intraosseous, hypertension, bursitis, tendinitis, and muscle spasm.
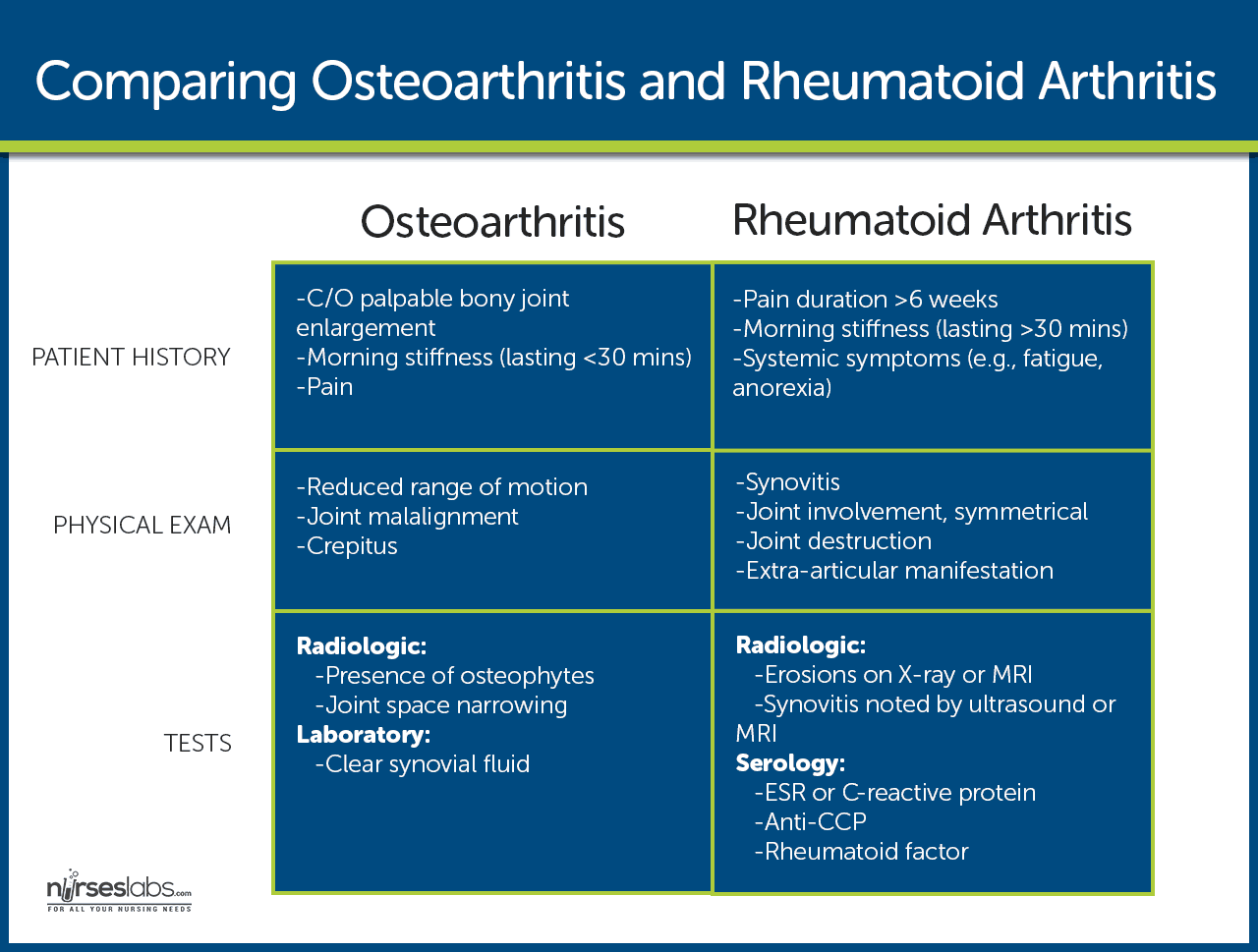
- Stiffness. Stiffness, which is mostly experienced in the morning or upon awakening, usually lasts less than 30 minutes and decreases with movement.
- Functional impairment. Functional impairment results from pain on movement and limited motion caused by structural changes in the joint. Stages of Osteoarthritis
Stage 0 – Normal
When the knee shows no signs of osteoarthritis, it is classified as Stage 0, which is normal knee health, with no known impairment or signs of joint damage.
Treatments
There is no treatment required for stage 0 OA.
Stage 1 – Minor
Stage 1 OA patients will develop very minor wear & tear and bone spur growths at the end of the knee joints. However, at this stage it is unlikely you will feel pain or discomfort.
Treatments
If the patient is not predisposed to OA, orthopedic physicians may not recommend any special treatment for stage 1. However, supplements such as glucosamine and chondroitin may be recommended. Lifestyle considerations like regular exercise may also prove to be helpful.
Stage 2 – Mild
In Stage 2, diagnostic images or X-rays of knee joints will show more bone spur growth, and though the space between the bones appear normal, people will begin experiencing symptoms of joint pain. Typically, the area around the knee joints will feel stiff and uncomfortable, particularly when sitting for an extended period, after rising in the morning, or after a workout. Though the cartilage and soft tissues remains at a healthy size, there is proteolytic breakdown of the cartilage matrix from an increased production of enzymes, such as metalloproteinases.
Treatments
When your physician detects and diagnoses OA at this early stage, it is easier to follow a plan to stop the progression of this joint disease. There are different nonpharmacologic therapies to help relieve the pain and discomfort caused in this mild stage. Many patients are recommended a strict regimen of exercise and strength training for increased joint stability. Additionally, braces, knee supports or shoe inserts may be used to protect the knee from stress.
Stage 3 – Moderate
Stage 3 is referred to as “moderate”, where there is obvious erosion to the cartilage surface between bones and fibrillation narrows the gap between the bones. There are proteoglycan and collagen fragments released into the synovial fluid as the disease progresses, wherein the bones develop spurs at the joints as it becomes rougher.
With the progression of osteoarthritis of the knee, there is obvious joint inflammation which causes frequent pain when walking, running, squatting, extending or kneeling. Along with joint stiffness after sitting for long or when waking up in the morning, there may be popping or snapping sounds when walking.
Treatments
Over the counter NSAIDs or pain-relief therapies may be prescribed. If these methods are not effective, the orthopedic doctor may prescribe stronger pain medicine, such as codeine and oxycodone.
Patients that have not responded positively to physical therapy, weight loss program, use of NSAIDs may require viscosupplementation, which are intra-articular injections of hyaluronic acid into the knee joint. Moderate knee arthritis can be treated aggressively with three to five injections of hyaluronic acid over 3-5 weeks’ time, which may take several weeks for the treatment to start showing results, but pain relief typically lasts six months.
Stage 4 – Severe
Stage 4 is considered to be severe. In stage 4 the joint space between the bones are considerably reduced, causing the cartilage to wear off, leaving the joint stiff. The breakdown of cartilage leads to a chronic inflammatory response, with decreased synovial fluid that causes friction, greater pain and discomfort when walking or moving the joint.
There is increased production of synovial metalloproteinases, cytokines and TNF that can diffuse back into the cartilage to destroy soft tissue around the knee. The advanced stage of the disease shows development of more spurs causing excruciating pain, which makes even everyday chores, including walking and descending stairs a challenge.
Treatments
In cases of severe OA of the knee, an option is performing osteotomy or bone realignment surgery, wherein the orthopedic surgeon cuts the bone above or below the knee to shorten the length and help realign it for less stress on the knee joint. This surgery helps protect the knee by shifting the weight of the body away from the site of the bone spur growth and bone damage.
Another surgical option is total knee replacement, or arthroplasty. During this surgical procedure, the damaged joint is removed and replaced with a plastic or metal prosthesis device. Recovery from surgery may take several weeks and requires patience and discipline, with continuous physical and occupational therapy to regain full mobility.
-
Prevention of Osteoarthritis
Although no treatment halts the degenerative process, certain preventive measures can slow the progress if undertaken early enough.
- Weight reduction. To avoid too much weight upon the joints, reduction of weight is recommended.
- Prevention of injuries. As one of the risk factors for osteoarthritis is previous joint damage, it is best to avoid any injury that might befall the weight-bearing joints.
- Perinatal screening for congenital hip disease. Congenital and developmental disorders of the hip are well known for predisposing a person to OA of the hip.
